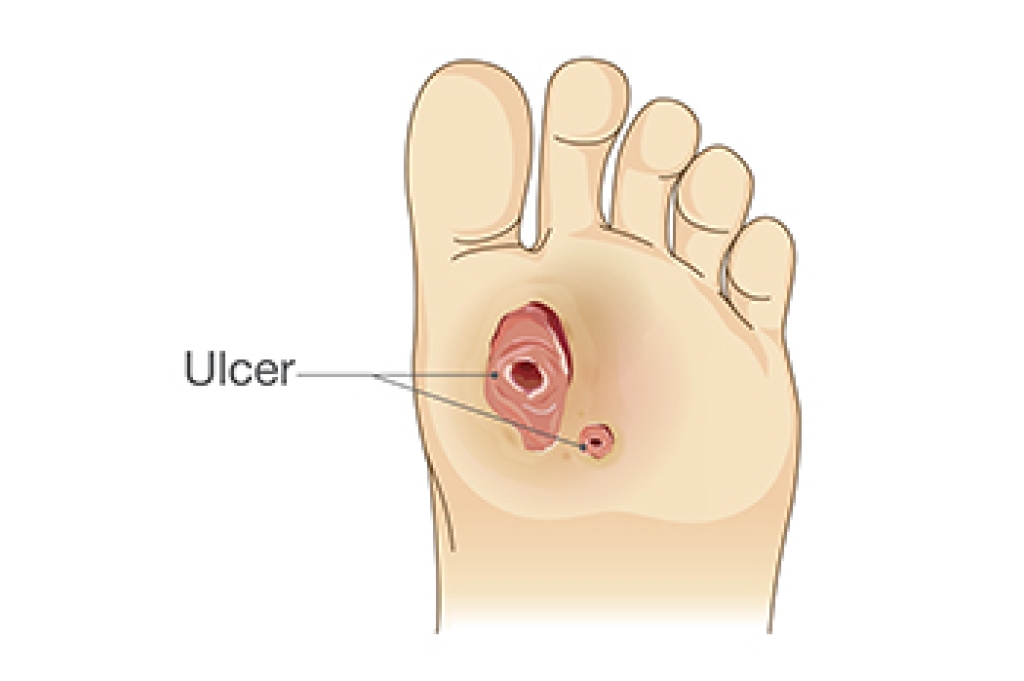
Diabetic foot ulcers are open sores that develop on the feet of individuals with diabetes, often forming on pressure points such as the heels or toes. These wounds progress through stages, beginning as redness or skin breakdown and advancing to deeper tissue involvement, if not treated. Causes include poor blood sugar control, neuropathy that reduces sensation, blood flow problems that slow healing, and improper shoes that create friction or pressure. Without proper care, ulcers can worsen and lead to serious complications. A podiatrist can help by assessing the wound, removing damaged tissue, improving pressure distribution, and guiding proper foot care to support healing. If you have diabetes and notice any signs of a foot ulcer, it is strongly suggested that you promptly schedule an appointment with a podiatrist who can help you to manage this serious condition.
Diabetic foot care is important in preventing foot ailments such as ulcers. If you are suffering from diabetes or have any other concerns about your feet, contact Judson Siegel, DPM from Assabet Family Podiatry. Our doctor can provide the care you need to keep you pain-free and on your feet.
Diabetic Foot Care
Diabetes affects millions of people every year. The condition can damage blood vessels in many parts of the body, especially the feet. Because of this, taking care of your feet is essential if you have diabetes, and having a podiatrist help monitor your foot health is highly recommended.
The Importance of Caring for Your Feet
- Routinely inspect your feet for bruises or sores.
- Wear socks that fit your feet comfortably.
- Wear comfortable shoes that provide adequate support.
Patients with diabetes should have their doctor monitor their blood levels, as blood sugar levels play such a huge role in diabetic care. Monitoring these levels on a regular basis is highly advised.
It is always best to inform your healthcare professional of any concerns you may have regarding your feet, especially for diabetic patients. Early treatment and routine foot examinations are keys to maintaining proper health, especially because severe complications can arise if proper treatment is not applied.
If you have any questions, please feel free to contact our offices located in Plainville, Marlborough, and Somerset, MA . We offer the newest diagnostic and treatment technologies for all your foot care needs.