Winter activities challenge the feet and ankles in ways that warm weather sports do not. Skiing, skating, and snowboarding can place sudden force on the lower joints, leading to sprains, tendon irritation, or bruising. Additionally, fractures can occur if a landing or turn goes wrong. Boots that are stiff or overly tight can cause pressure points, while icy surfaces increase the chance of slipping and twisting the ankle. Cold temperatures also make muscles less flexible, which can reduce stability and slow reaction time. When discomfort develops, early care helps prevent a minor issue from turning into something more serious. A podiatrist can assess swelling, tenderness, or difficulty bearing weight, and determine which structures are involved. This foot doctor can also recommend protective footwear or supportive inserts, as well as offer targeted treatment to promote healing. If winter activities leave you with lingering foot or ankle pain, it is suggested that you see a podiatrist for effective relief solutions.
Sports related foot and ankle injuries require proper treatment before players can go back to their regular routines. For more information, contact Judson Siegel, DPM of Assabet Family Podiatry. Our doctor can provide the care you need to keep you pain-free and on your feet.
Sports Related Foot and Ankle Injuries
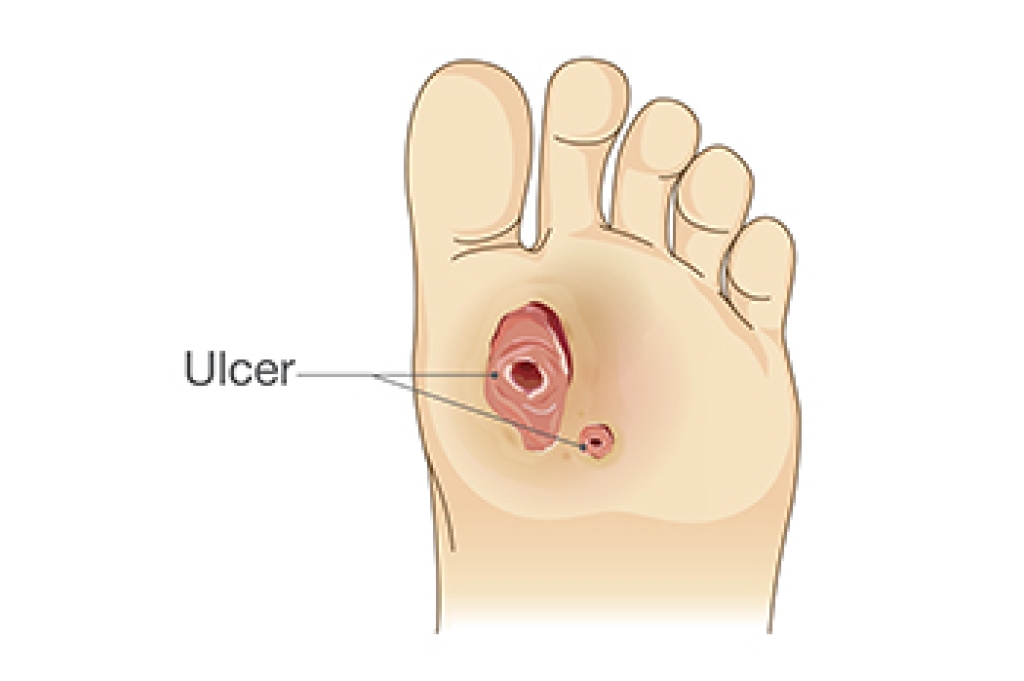
Foot and ankle injuries are a common occurrence when it comes to athletes of any sport. While many athletes dismiss the initial aches and pains, the truth is that ignoring potential foot and ankle injuries can lead to serious problems. As athletes continue to place pressure and strain the area further, a mild injury can turn into something as serious as a rupture and may lead to a permanent disability. There are many factors that contribute to sports related foot and ankle injuries, which include failure to warm up properly, not providing support or wearing bad footwear. Common injuries and conditions athletes face, including:
- Plantar Fasciitis
- Achilles Tendinitis
- Achilles Tendon Rupture
- Ankle Sprains
Sports related injuries are commonly treated using the RICE method. This includes rest, applying ice to the injured area, compression and elevating the ankle. More serious sprains and injuries may require surgery, which could include arthroscopic and reconstructive surgery. Rehabilitation and therapy may also be required in order to get any recovering athlete to become fully functional again. Any unusual aches and pains an athlete sustains must be evaluated by a licensed, reputable medical professional.
If you have any questions please contact our offices located in Plainville, Marlborough, and Somerset, MA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.